Discover a Minimally Invasive Procedure Transforming the Treatment of Chronic Low Back Pain
(NAPSI)—For more than half of her life, 43-year-old Megan Bettor dealt with bouts of excruciating low back pain. She doesn’t remember a specific accident or injury that caused the initial pain – all she knows is that it was a constant part of her life.
Megan’s pain was centered in her lower back and was aggravated by sitting, bending forward or with physical activity. For many years, she managed it with conservative treatments such as over-the-counter medications and physical therapy.
As the pain worsened, these treatments stopped working. When this interior designer and mom of two wasn’t busy, she often found herself spending weekends laying in bed unable to move due to her pain.
“There wasn’t just like a bad week,” said Megan. “It was every day, every morning [where it was] nearly impossible to get out of bed, brush my teeth and feed our dog.”
Megan knew something had to change and began exploring surgical options, including a disc replacement, an invasive and expensive treatment that may or may not address her pain.
That’s when she met Ramana Naidu, M.D., director of pain management, MarinHealth Medical Center and interventional pain physician and anesthesiologist. Dr. Naidu not only offered Megan a clear diagnosis of vertebrogenic pain but also a proven treatment.
The ABCs of vertebrogenic low back pain
After examining Megan’s symptoms, Dr. Naidu reviewed an MRI of her low back. He identified specific changes in her vertebral endplates, called Modic changes, that indicated she likely had vertebrogenic low back pain.
This type of pain is a relatively new discovery and caused by vertebral endplates that get damaged due to age, wear, tear and everyday living. While approximately 5.3 million people in the U.S. are living with vertebrogenic pain1, this condition did not have an official diagnosis until recently, let alone a treatment.
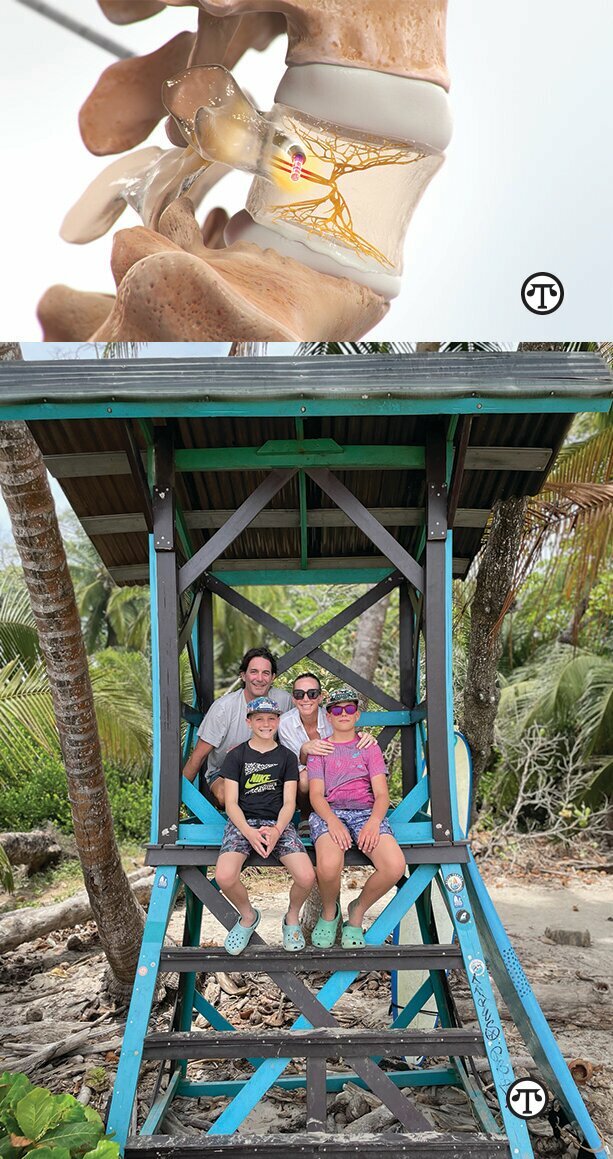
Dr. Naidu thought Megan would be an ideal candidate for a procedure utilizing Boston Scientific’s Intracept™ Intraosseous Nerve Ablation System, which provides a minimally invasive, same-day treatment specifically designed to address vertebrogenic pain.
“Patients with vertebrogenic pain are the same type of low back pain patients we have seen for years,” said Dr. Naidu. “The frustration we had as providers is that we could identify these patients but there was little we could do to effectively treat them. The Intracept system changed that.”
The Intracept system targets a specific nerve in the lower back—the basivertebral nerve or BVN—that transmits pain signals from the damaged vertebral endplates to the brain. The Intracept system uses a radiofrequency probe to heat the BVN and prevent it from sending these signals. The procedure is proven to be safe and effective2, with patients reporting significant pain and functional improvements at five years after a single treatment.3
“Historically, the disc was presumed to be the source of most chronic low back pain, but recent research demonstrates that the vertebral endplates play a significant role in causing pain,” said Ray Baker, M.D., vice president and chief medical officer, Neuromodulation, Boston Scientific. “By targeting the BVN, patients can achieve durable relief through a minimally invasive procedure.”
Regaining a life without vertebrogenic pain
After receiving insurance approval, Megan underwent her procedure with the Intracept system in November 2023. Her pain relief was immediate and, as time went on, Megan ramped up her physical activities without the accompanying low back pain.
Soon she found herself traveling with her family, including on trips to ski and surf – something she wouldn’t have dreamed of doing before. It also gave her an opportunity to appreciate doing the little things that previously would have caused her pain.
“Intracept saved my life,” said Megan. “That sounds dramatic but it’s the most significant thing that could have happened to me.”
For Dr. Naidu, outcomes like Megan’s inspire him to continue educating his patients and the broader medical community on vertebrogenic pain and the Intracept system.
“If she had surgery, it might have been helpful, but what would the long-term consequences have been? With Intracept, you don’t have to worry about long-term consequences,” said Dr. Naidu. “That’s why this therapy is so special – it’s really changing people’s lives in a major way.”
Find an Intracept-trained physician near you
If you have suffered from chronic low back pain for at least six months and find it gets worse with physical activity, you may have vertebrogenic pain.
Physicians across the US are trained to make this specific diagnosis and to determine if treating your low back pain with the Intracept system may be an option for you. You can also use the Intracept Physician Finder to locate a physician near you to make an appointment and learn more about this diagnosis and proven treatment.
1 Hoy D, March L, Brooks P, et al. The global burden of low back pain; estimates from the Global Burden of Disease 2010 study. Annals of the Rheumatic Diseases 2014;73:968-974. https://ard.bmj.com/content/73/6/968;The global point prevalence of LBP was 9.4% (95% CI 9.0 to 9.8), (333M U.S. pop * 9.4% = 31M); Lorio et al. International Journal of Spine Surgery December 2022, 16 (6) 1084-1094; DOI: https://doi.org/10.14444/8362;http://www.ijssurgery.com/content/16/6/1084; estimated that 15% of CLBP patients suffer from primary vertebrogenic pain.
2 Koreckij T, Kreiner S, Khalil JG, Smuck M, Markman J, Garfin S. Prospective, randomized, multicenter study of intraosseous basivertebral nerve ablation for the treatment of chronic low back pain: 24-month treatment arm results. NASSJ. Published online October 26, 2021. DOI: https://doi.org/10.1016/j.xnsj.2021.100089
3 Fischgrund J, Rhyne A, Macadaeg K, et al. Long-term outcomes following intraosseous basivertebral nerve ablation for the treatment of chronic low back pain: 5-year treatment arm results from a prospective randomized double-blind sham-controlled multi-center study. Eur Spine J. 2020;29(8):1925-34. doi.org/10.1007/s00586-020-06448-x
Results from case studies are not necessarily predictive of results in other cases. Results in other cases may vary.
Word Count: 936
Keywords
chronic back pain, physical activity, sitting, bending, vertebrogenic, low back pain, doctors, surgery, vertebrae, spine, Intracept Intraosseous Nerve Ablation SystemComments